LSD lovers are an organized bunch. I’m seated among dozens of them at Neuehouse, a members club in Midtown Manhattan, and though their Tibetan grounding bracelets click and clack, the group itself is relatively quiet, save a woman behind me recounting her most recent trip. “I did it with a healer,” she recounts to a friend. “The healer said, ‘Drop into your inner voice,’ and I’m like, ‘Which one?!’ It took a minute.”
We’re gathered here for “Psychedelics Now,” a panel exploring the benefits and limits of mind-altering substances for medical purposes, as well as issues like ADHD and creative blocks.
Were there a few moments when I wondered if I was hearing my dad’s old stories from Berkeley instead of a meditation on the future of mental health? Absolutely, especially considering there was a guest appearance from drug lord William Leonard Pickard, aka “The Acid King,” who allegedly produced 90 percent of all LSD on earth. (He reads a short story based on an accidental acid overdose at the top of a mountain, with lines like, “I prayed in a timeless void, for it was the moment of death and rebirth...the ultimate vision was our own mundane, magical world.”)
But there were also too many useful scientific facts and proven trials to ignore. So if you’re thinking about exploring psychedelics for help with depression, anxiety, or even chronic pain, here’s a starter pack on what you should know. (Disclaimer: Talk to your doctor before potentially considering psychedelics as treatment.)
You’ve probably already used a psychedelic, even if you didn’t realize it.
“A psychedelic is anything physical that manifests in the mind,” says Dr. Julie Holland, the author of Good Chemistry and Moody Bitches. “MDMA, otherwise known as ecstasy or molly? That’s a psychedelic.” Dr. Holland also counts meditation as a form of psychedelics, even though it’s not chemical, along with LSD, “magic” mushrooms, some strains of cannabis, and ketamine.
Psychedelics are chemical shortcuts to your “inner child.”
“When you ask, ‘Can you rewire the brain?’ you actually can with psychedelics,” Dr. Holland says. “These compounds enhance neuroplasticity…which is the part of the brain that sets patterns and reactions in the nervous system.” Turns out natural neuroplasticity is greatest in infancy and childhood, when attachment patterns are set with caregivers and the wider world—and, yeah, sometimes that can cause big problems. Psychopharmacologists think psychedelics are part of the solution to “treatment-resistant” forms of depression and PTSD that require more than therapy and mood-enhancing pills.
You’ll need—and want—a psychiatric evaluation to legally take them.
Nushama is a legal Psychedelic Wellness Center in New York City that uses ketamine as a form of intense psychotherapy. To get it, you’ll need to first undergo lengthy medical and psychiatric evaluations to ensure the drugs do more good than harm in your system. “Most people pass,” says Jay Godfrey, the “recovering fashion designer” who co-founded the space. But people living with schizophrenia, bipolar disorder, and manic episodes may not be the best fit for ketamine, along with those taking certain drugs for hypertension, anxiety, and ADHD—so do this with a doctor, not a friend at a warehouse party.
Breakdowns happen.
“Psychedelics can release the brain from a fear-based pattern,” explains Dr. Gita Vaid, a member of Mount Sinai’s Psychedelic Psychotherapy Research and Trauma Center. “They don’t just confront the symptom; they get behind the symptom.” With medical-grade ketamine specifically, Dr. Vaid warns, “You can get into a lot of trouble. We have to be really careful.” (One more time for the people in back: Only do these drugs with a licensed doctor!) More often, Dr. Vaid reports seeing breakdowns leading to breakthroughs. “Sometimes even one session can lessen depression,” she explains, “because your brain is finally letting go of the fear that’s blocking you from fully participating in the world.”
It costs the same as a Chanel bag.
“These are not inexpensive,” concedes Neil Markey, a combat war veteran who now facilitates legal psilocybin (“magic mushroom”) at Beckley Retreats in Jamaica. Ketamine cycles at Nushama cost about $4500, with most insurance plans still lagging behind in treatment funding. “Access is still a huge problem,” says Dr. Holland, noting that donations to programs like MAPS (the Multidisciplinary Association for Psychedelic Studies) are trying to make up the treatment gap until politicians approve more funding. “We can also keep the cost down by doing sessions in group settings,” says Markey, “Which to me, is the way humans are meant to heal. These substances have always been done in community. We’re supposed to do this work as a group.”
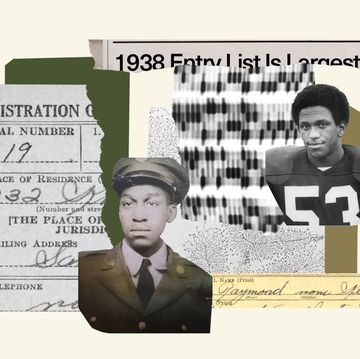
You can’t talk about psychedelics without talking about prison reform.
Pickard spent 20 years in federal prison before being granted compassionate release thanks to lobbyists and public pressure. Thousands more are still incarcerated for drugs that are now legal and medically recognized. Those imprisoned are disproportionately Black and brown, and without their release, psychedelic medicine will remain a privilege built on the backs of our fellow Americans. Learn more at The Sentencing Project, continue asking your local leaders where they stand on prison and drug reform, and ensure your own psychedelic experience gives reparations (read: money) to those incarcerated for the same drugs now being used as tools for healing the 1 percent.
This might be a way out of the opioid crisis.
Wait, these drugs can treat addiction to other drugs? Definitely maybe. “The system has failed so many people,” says Godfrey. “Now we’re seeing data that shows psychedelics helping with [opioid] withdrawal symptoms and addiction issues.” A recent Harvard study notes 30 percent less opioid dependence among magic mushroom users, while smaller studies in New Zealand note ibogaine—which comes from tree roots from the West African rainforest—has significantly decreased relapses among those in recovery.
Psychedelics aren’t necessarily a forever thing.
“We do not want you dependent on medicine,” Markey insists, saying that although psychedelics can help accelerate one’s mental health journey, “they don’t work without lifestyle changes” proven to boost one’s mood like meditation, hydration, and even just spending more time outside. (Scientists recommend an average of 17 minutes a day.) “Recreation is also therapy,” says Dr. Holland. “We believe in psychedelics as a path to healing. But healing itself is mind, body, soul—it’s everything already inside of you that just needs to be more connected.”